A Manchester hospital is providing a ground-breaking treatment for sickle cell costing £1million per patient, according to a lead specialist nurse.
The Manchester Royal Infirmary (MRI) is treating its first patient with gene-editing therapy, a procedure that could cure sickle cell disease for £1,651,000 per patient.
The new one-off treatment, called exagamglogene autotemcel, edits a patient’s blood stem cells to correct the genetic defect.
Chelsea Soka is the lead haemoglobinopathy specialist nurse at the MRI, the first hospital in the UK to have a sickle cell unit.
She said: “The criteria for gene therapy is quite rigid and quite strict so it won’t be eligible to people just for the sake of it.”
Sickle cell disease is a genetic condition that causes red blood cells, which are normally round and flexible, to become stiff, sticky and crescent-shaped.
A sickle cell crisis is when the crescent-shaped red blood creates blockages within blood vessels causing severe pain.
A crisis can happen anywhere in the body.
The new gene-editing procedure includes doctors collecting the patient’s stem cells, modifying them in a lab then infusing them back into the patient after they have done a round of chemotherapy.
NHS clinical trials found all patients who received the one-off treatment avoided hospitalisation for a year following the procedure — and also 98% had still avoided hospitalisation around 3.5 years later.
Soka said: “It’s quite extensive and it puts your body through a lot so the disease burden has to be severe.
“The patient needs to not have had any strokes which rules out quite a few people unfortunately.
“Their liver has to be moderately okay. They can’t have any issues with their liver through their sickle cell.”
The gene-editing treatment was approved last year for use on the NHS in England for older children and adults that have recurrent crises and lack a stem cell donor.
The treatment is only available at specialist NHS centres in London, Manchester and Birmingham.
Only around 50 patients a year are expected to benefit from the £1million procedure.
Most people with sickle cell manage their crises at home, with patients usually seeking hospital care only if the pain is uncontrolled, according to the National Institute for Care Excellence (NICE).
Sybil Asa is a 22-year-old trainee solicitor with sickle cell.
She said: “If I’m experiencing a crisis my last resort is going to the hospital because the treatment is bad.
“If you’re not in a hospital that knows how to deal with sickle cell then you’re probably going to get the worst treatment ever.”
A 2025 NHS Race and Health Observatory report found that sickle cell patients managed an average of seven painful crises without medical help in the past year.
Asa said: “I would describe the pain to someone who doesn’t have sickle cell as the worst pain you could possibly experience.
“It’s like 1,000 needles or pins squeezing your body and you can’t stop it.
“It’s not something you can describe in words because it is honestly just that painful.”
In the report, patients found a lack of awareness from A&E staff resulted in delays in receiving treatment and sub-standard care.
Asa said: “I had a crisis in my leg once so I couldn’t walk at all.
“I had to call for assistance for 10 minutes just for them to come and help me to go to the toilet.
“I think they just disregard you and sort of think that you’re attention-seeking just because they don’t know how to deal with your pain.”
There are around 17,000 people living with this sickle cell disease, making it one of the country’s most common genetic disorders.
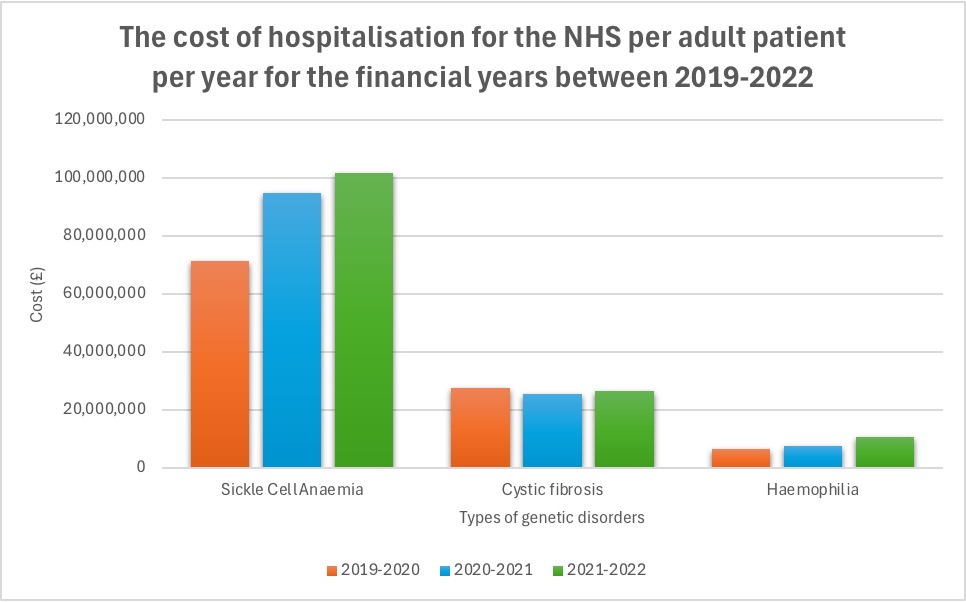
Treating sickle cell anaemia in adults costs the NHS annually an average of £89,386,224 per patient hospitalisation between 2019-2022, according to the 2025 NHS Race and Health Observatory report.
This is more than three times the average cost to treat cystic fibrosis, another inherited genetic disorder.
In England, there are only 0.5 specialist nurses per 100 sickle cell patients compared with two per 100 for cystic fibrosis patients, according to NICE.
As the lead specialist haemoglobinopathy nurse at MRI, Soka’s work focuses on genetic disorders that affect the blood.
Soka said: “We still face the same issues such as a lot of people not really understanding what sickle cell number one is.
“It’s a medical emergency that needs to be treated within 30 minutes.
“It was very hit and miss, even in major cities like London and Manchester.”
According to the 2025 report, 49% of sickle cell patients reported that healthcare professionals were not completely sympathetic and understanding in an emergency care setting.
Soka said when sickle cell patients arrived at A&E with a seemingly normal presentation, some healthcare professionals would have the mentality of getting to the patients when they got to them.
She said: “That is completely wrong because people mask pain differently.
“I’ve had a patient who sings to distract himself from the pain.
“Someone may say he’s not in much pain if he can sing, which is wrong.
“You wouldn’t tell a pregnant lady they weren’t in pain after a caesarean.”
A spokesperson for NHS England said: “The waiting list fell by more than 86,000 in November to 7.31 million – and the milestone comes a year since the publication of the Elective Reform Plan.
“The progress came despite the NHS’s busiest ever year, with 27.8 million A&E attendances in 2025 – up by over 367,000 on 2024, with 2.33 million attendances in December alone.
“In December, 73.8% of patients were seen within the 4-hour A&E target – 50,000 higher than a year earlier.”
Featured image credit: Jafar Ahmed via Unsplash





Join the discussion